د. رمضان جلال شمس الدين
استشاري جراحة المخ والاعصاب والعمود الفقري بالهيئة العامة للمستشفيات والمعاهد التعليمية .
عضو الجمعبة المصرية لجراحى المخ والاعصاب .
عضو الجمعية المصرية لجراحى العمود الفقري .
عضو جمعية الشرق الاوسط لجراحة العمود الفقري .
له العديد من الابحاث الدولية المنشورة فى مجال التخصص .
استشاري الجراحات الميكروسكوبية لاورام المخ وقاع الجمجمة.
اسشتاري جراحات العمود الفقري .
استشاري جراحة اعصاب الاطفال .
أحجز موعد
قم بارسال رسالتك
تواصل مع دكتور رمضان
تواصل معنا
+201006707137البريد الإلكتروني
info@dr-ramadanshamseldien.comحداب العمود الفقري - وطرق التعافي منه
Introduction for kyphosis
Kyphosis, a condition characterized by an excessive outward curvature of the spine, has become a topic of increasing concern in our sedentary lifestyle era. This comprehensive guide aims to demystify kyphosis, addressing its various forms, causes, treatment options, and preventive measures. We will explore everything from the basics of what kyphosis is, to detailed discussions on surgical and non-surgical treatments, ensuring a thorough understanding of this spine condition.
What is Kyphosis?
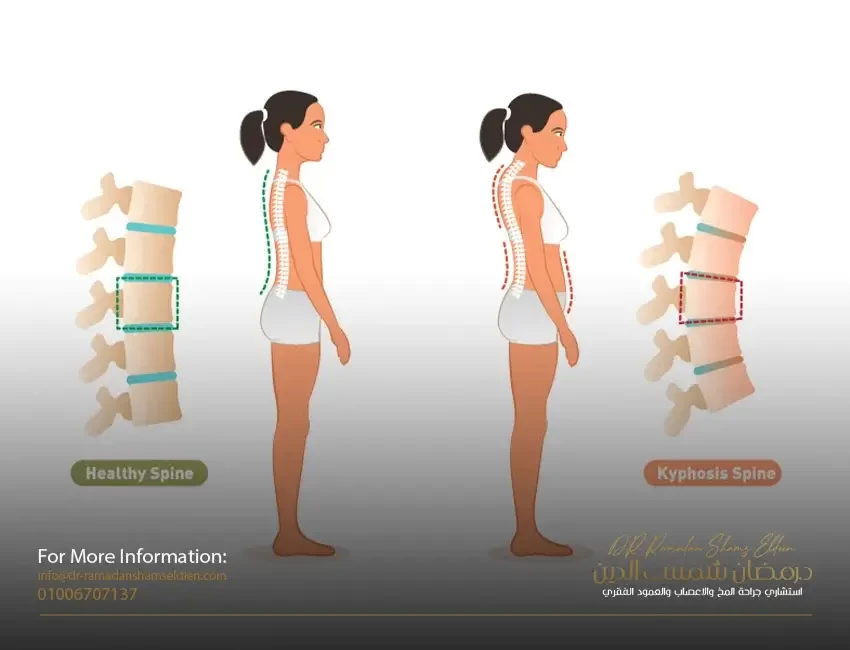
Defining Kyphosis
Kyphosis is a spinal disorder where an abnormal curvature forms, causing a hunchback or slouching posture. It can occur at any age but is most common in older adults, particularly women. While a certain degree of curvature is normal, kyphosis refers to an exaggerated curve that can lead to various health concerns.
Types of Kyphosis
There are several types of kyphosis, but two notable ones are:
- Lumbar Kyphosis: This type involves the lower back, leading to a forward curvature that's less common but equally concerning.
- Kyphotic Spine: A general term that refers to any section of the spine affected by this excessive curvature, most commonly seen in the thoracic (upper) spine.
H3: Common Confusions
It's not uncommon to come across the term "kyposis." It's important to clarify that "kyposis" is a common misspelling of kyphosis and refers to the same condition.
Causes and Genetics of Kyphosis
Exploring the Causes
Kyphosis can stem from various factors, including degenerative diseases (like arthritis), disc degeneration, osteoporosis, trauma, or even poor posture over time. In some cases, it's present from birth due to a malformation of the spine or develops during adolescence due to unknown reasons (Scheuermann's disease).
Genetic Factors
Is kyphosis genetic? While lifestyle and environmental factors play significant roles, genetics can contribute, especially in cases like congenital kyphosis. However, having a family member with kyphosis doesn't guarantee you'll have it, but it may increase your risk.
Kyphosis in Adults
Adult vs Juvenile Kyphosis
While kyphosis can affect individuals at any age, its presentation and implications differ between adults and juveniles. In adults, kyphosis often results from conditions like osteoporosis, degenerative spine disease, or muscle weakness. It can lead to pain and mobility issues, significantly impacting quality of life. In contrast, juvenile kyphosis, particularly Scheuermann's disease, often arises during the growth spurt before puberty and may correct itself over time or require intervention if severe.
Identifying Kyphosis
Signs and Symptoms
Recognizing kyphosis involves looking for signs such as a visible hump on the back, pain in the spine, stiffness, and in severe cases, difficulty breathing due to the compression of internal organs. Pain may become more pronounced during long periods of standing or sitting.
H3: Visual Guide
To aid in identification, visual references such as kyphosis pictures can be helpful. These images typically show the noticeable curvature from the side, providing a clear contrast to a normal spine's appearance.
Kyphosis Treatment Methods
Overview of Treatments
Treatment for kyphosis varies depending on the severity and underlying cause. Options range from conservative methods like physical therapy and medication to more invasive procedures like surgery. The primary goals of treatment are to reduce pain, improve function, and prevent the curvature from worsening.
Corrective Measures
Non-surgical methods to fix kyphosis include:
- Physical Therapy: Exercises to strengthen back muscles and improve posture.
- Bracing: In some cases, especially in adolescents, wearing a brace can help correct spinal curvature.
- Medications: Pain relievers and anti-inflammatory drugs can help manage symptoms.
Kyphosis Surgery
Surgical Options
Surgery is usually reserved for severe cases of kyphosis where the curvature is significantly impacting the patient's quality of life or health. Procedures may involve spinal fusion, where vertebrae are joined together to stabilize the spine, and osteotomy, where a portion of the bone is removed to correct the alignment.
Before and After Surgery
The comparison of kyphosis surgery before and after can be dramatic, showing significant improvement in the spine's alignment. However, it's crucial to have realistic expectations and understand that surgery involves risks and a considerable recovery period.
Non-Surgical Approaches
Physiotherapy and Exercises
Specific exercises can help manage kyphosis by strengthening the back muscles and improving posture. A physiotherapist can design a personalized exercise program suited to the individual's condition.
Lifestyle Adjustments
In addition to exercises, making lifestyle changes can be beneficial. These include maintaining a healthy weight, ensuring adequate nutrition (particularly calcium and vitamin D for bone health), and practicing good posture.
Living with Kyphosis
Managing Pain
Living with kyphosis can often mean managing varying degrees of back pain. Pain management strategies include regular physical therapy, over-the-counter pain relievers, and, in some cases, prescription medications. Heat therapy and relaxation techniques can also be beneficial for reducing discomfort and improving muscle function.
Quality of Life
Kyphosis can impact quality of life, not just physically but also emotionally and socially. It's important for individuals to seek support, whether through therapy, support groups, or community resources. Adjusting daily activities to accommodate physical limitations and focusing on activities that bring joy and fulfillment can also help in maintaining a positive outlook.
Preventing Kyphosis
Prevention Strategies
While not all forms of kyphosis can be prevented, certain measures can reduce the risk or lessen the severity. These include maintaining good posture, engaging in regular exercise, especially activities that strengthen the back and core muscles, and ensuring proper nutrition for bone health.
The Importance of Early Detection
Early detection of kyphosis is crucial for effective management. Regular check-ups, especially during the adolescent growth spurt, can help in identifying any abnormal spine curvatures early on. Early intervention can often prevent the progression of kyphosis and reduce the need for more invasive treatments in the future.
Conclusion
Kyphosis, with its various forms and implications, requires a comprehensive understanding for effective management and treatment. From identifying the early signs to exploring treatment options and coping strategies, this guide aims to provide a thorough overview of kyphosis. However, it's important to remember that each case is unique, and what works for one person may not work for another. Consulting with healthcare professionals, staying informed, and being proactive about spine health are key to managing kyphosis effectively.
الإنزلاق الغضروفي القطني والآم اسفل الظهر
Lumbar herniated disc and lower back pain
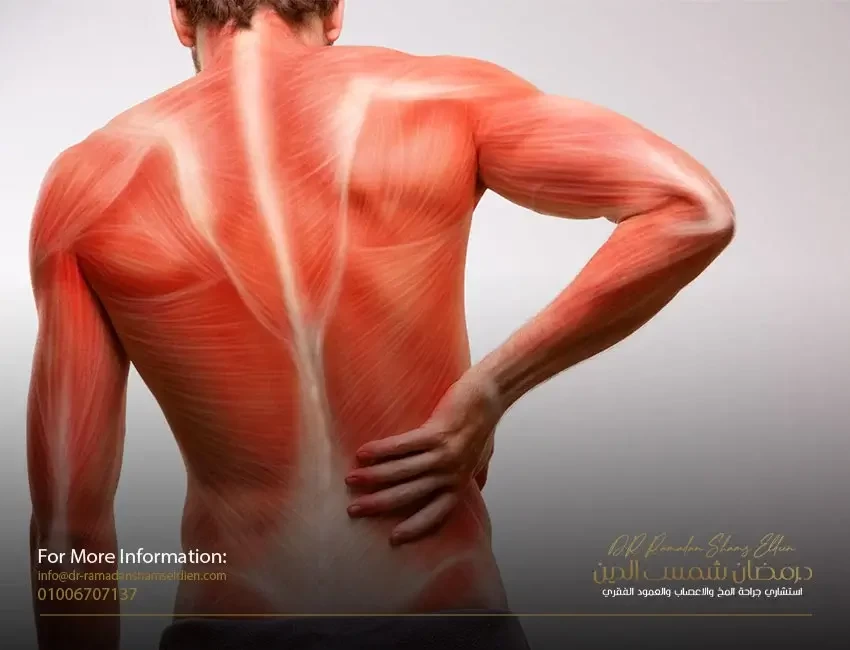
Low back pain is one of the most common disorders affecting the musculoskeletal system and is considered the most prevalent in the modern era. It still poses a real health challenge in terms of prevention and treatment, and it ranks third in terms of the high cost of treatment after cardiovascular diseases and cancerous diseases.
The spine is the only longitudinal axis of the body that bears the entire weight of the trunk, and its lumbar vertebrae are connected with the pelvis and its movement with the sacral vertebrae, and accordingly, any imbalance that affects the body axis (functionally or anatomically) will negatively affect the functional level of the trunk and the movement of the body in general and thus It may reduce psychological, economic and social efficiency, especially when pain appears, which greatly affects the daily activities of the individual and the quality of life he lives. In dispersing the forces acting on it by distributing pressure on the nucleus of the cartilaginous disc, which distributes it equally on the surrounding cartilage rings in all directions over the entire area of the cartilaginous disc. The vertebral congruence condition becomes lost.
Low back pain is usually divided in terms of recurrence into acute, which occurs suddenly and often occurs once or twice in life, and chronic, which occurs frequently, cumulatively and with a higher level of severity with each time.
It is divided in terms of the type of cause into specific mechanical pain, which is directly related to the pain that results from acute muscle strain and herniated disc, which is responsible for 90% of these cases, and to non-mechanical, non-specific pain, which is indirectly related to the pain that results from anxiety states, enlargement of the prostate gland, and dryness. Herniated disc. In terms of the degree of pain, it is divided into simple, medium and severe pain.
A herniated disc (herniated disc or lumbar disc herniation) is defined as the nucleus and its rings being pushed irregularly from between the vertebrae to the back under the influence of severe pressure with the occurrence of a hernia in the cover of the cartilaginous rings, to grow towards the back to enter the spinal canal and put pressure on the spinal cord. This is called this The condition of the central compressive cartilage. Either it grows backward and to one side and presses on one of the nerve roots branching from the spinal cord. This condition is called the noncentral or lateral compressive cartilage. Regardless of the type of herniated disc or herniated disc in the lumbar disc, it causes severe defensive muscle contractions.
The range of motion between the vertebrae is reduced, in addition to the occurrence of severe pain, and the level of danger is high, as in road accidents, for example, where the pressure is very strong to cause a cartilage rupture with sharp ends that threaten to tear and injure the surrounding tissues and nerves during movement, causing partial or total paralysis of the nerve depending on the force of pressure The severity of the injury to the nerve root.
The most frequent cases are in the lumbar region between the fourth and fifth lumbar vertebrae and between the fifth lumbar and first sacral vertebrae.
Often, these patients complain of a group of severe neurological disorders represented by sensory impairment and disturbance in
The level of the reflex reaction, weakness in the muscular ability of the lower extremities or one of them, and severe pain in the direction responsible for the nerve root compressed in the herniated disc, which makes this disease a major cause to change the nature of the patient’s psychological, social, economic and family life, especially when it causes any degree of partial or partial disability. total
As for recurrent chronic cases, it is accompanied by a group of functional and anatomical changes on the lower back before the injury of a herniated disc, such as the occurrence of simple long-term muscle tension for many reasons. The cartilage disc reduces the concentration of water in that part of the cartilage, as water - despite its low concentration in the cartilage - plays an essential role in the process of distributing and spreading nutrients within the tissue of the lumbar disc and the speed of completion of vital reactions. With the persistence of muscle tension and the passage of time, this condition is called degenerative lumbar disc dehydration
Then begins a process of functional changes at the level, slowing down the speed of biochemical reactions, as well as anatomical changes in the formation of the lumbar disc, such as a lack of cartilage tissue cohesion and weakness in its elasticity and a decrease in the size and mass of the lumbar disc, so it becomes less able to absorb the forces acting on it, and the process of fibrosis of the spinal canal begins. The nerve roots exits increasingly over time to cause what is known as neural tube stenosis.
This results in sharp pains in the lower back extending to the lower extremities or one of them, with lethargy and weakness and a decrease in the ability to walk because of this, and the ability to straighten the trunk is weakened due to the contact of the cartilaginous protrusion with the nerve roots emerging from the spinal cord.
Most cases of herniated discs of the lumbar disc usually occur between the ages of twenty and forty, with most injuries occurring.
Due to improper lifting of heavy weights or injuries resulting from practicing some sports such as weightlifting and gymnastics, or for former athletes in some sports.
Herniated disc pain is treated medically
With it on the basis of removing the pressure from the cartilage of the cartilage
On the nerves by using the abduction tension
(slitting the vertebrae apart) naturally using positions
body (positional therapy) called stretching
ما هو مرض الجنف؟ وأنواعه وأشهر الأعراض
scoliosis
Scoliosis is a three-dimensional deformity of the spine and rib cage. It may develop as a single primary curve (looks like the letter C) or as two curves (a primary curve with a compensating secondary curve forming an S shape). Scoliosis may occur only in the upper back (thoracic) or lower back (lumbar), but it most commonly develops in the area between the thoracic and lumbar (the thoracic and lumbar areas). The doctor attempts to identify scoliosis by the shape, location, direction and size of the curve and, if possible, the cause. The severity of scoliosis is determined by the extent of the curvature of the spine and the angle of rotation of the trunk.
Determining and classifying the type of scoliosis often by the shape of the curve, by its location, or by its direction:
Scoliosis is classified according to the shape of the curve into structural (in other words true organic) or non-structural (which is functional or secondary). • In structural scoliosis, not only do the spine bend from side to side, but the vertebrae also rotate, resulting in a twisting of the spine . During torsion, one side of the rib cage is pushed out so that the spaces between the ribs widen and the shoulder blade protrudes (which causes the rib cage to deform or protrude); The other half of the rib cage is twisted inward, putting pressure on the ribs. • The non-structural or functional curve does not twist, but is a simple curve from side to side, and it is usually a compensation for the main structural curve or due to muscle spasms or other diseases of the vertebrae.
Determine scoliosis by its location. The location of the skeletal curve is determined by the location of the apical vertebra, which is the protruding vertebra at the apex (the highest point) of the spinal tuberosity. This particular paragraph will also undergo severe rotation.
Definition of scoliosis according to its direction. The direction of the curve in structural scoliosis is determined by whether the convex (rounded) side of the curve curves to the right or left. For example, a doctor defines a specific condition as right thoracic scoliosis if the apical vertebra is in the thoracic region (upper back) of the spine and the curvature is to the right.
The size of the curve is determined by taking length and angle measurements of the curve in an X-ray view.
Causes of scoliosis
First: idiopathic scoliosis
In 80% of patients, the cause of scoliosis is unknown. These conditions are called idiopathic scoliosis. Most cases of idiopathic scoliosis have a genetic basis, but researchers have not yet identified the gene or genes responsible for it. Researchers are investigating potential physical abnormalities that may cause bone or muscle imbalances that can lead to scoliosis. Among them are the following: muscles around the vertebrae. Some research suggests that imbalances in the muscles around the vertebrae may make children susceptible to spinal deformities as they grow. High arches in the feet. One study showed a higher incidence of abnormally high arches in the feet of people with idiopathic scoliosis, suggesting that altered balance may be a factor in some cases. Coordination problems. Some experts are looking at inherited impairments in cognition or coordination that may cause asymmetric spine development in some children with scoliosis. The investigators are also looking at possible abnormalities in collagen, an important structural protein found in muscle and bone. Other researchers are looking at a possible defective gene responsible for the production of fibrillin, an important component of the connective tissue that makes up bone and muscle. Some research has revealed abnormalities in a calcium-binding protein, calcodulin, among patients with scoliosis compared to the general population. Other researchers are still studying melatonin, a hormone secreted in the brain involved in sleep and growth. Animal studies and some human studies have found abnormalities associated with scoliosis.
Second: congenital scoliosis
Congenital scoliosis is caused by congenital abnormalities of the spine that usually involve abnormalities in the development of the vertebrae (missing or fused vertebrae). The condition usually appears around the age of two or between the ages of 8 and 13 as the spine begins to grow more rapidly, putting more stress on congenital malformations. Curves in such cases should be closely monitored, as they can progress rapidly. (Kidney problems, especially with only one kidney, often coincide with congenital scoliosis.)
Third: Scoliosis caused by genetic and medical disorders
Scoliosis may also be the result of muscle paralysis or deterioration from conditions such as myasthenia gravis, polio, or cerebral palsy. Other diseases that can cause scoliosis are Marfan syndrome, Friedreich's ataxia, Albers-Schönberg disease, rheumatoid arthritis, and osteogenesis imperfecta. Spinal cord injury may also cause scoliosis. A very rare genetic disease called familial dysautonomia has been identified as a cause of scoliosis in Jewish children of Ashkenazi descent. (It should be noted that only 500 cases have been reported globally, and this is related to the nature of the family composition of the Jews). Birth defects known to cause scoliosis include spina bifida or myelomeningocele (congenital hernia of the central nervous system).
Fourth: tumors of the vertebral column
Tumors and small growths or abnormalities in the spine may play a larger role than previously thought in the causes of scoliosis in young children. Back surgery to remove benign tumors increases the risk of spinal deformity.
Fifth: Causes of scoliosis other than structural or functional
Nonstructural scoliosis is sometimes caused by poor posture, leg length differences, and muscle spasms.
Scoliosis risk factors
General risk factors for idiopathic scoliosis. Idiopathic scoliosis (where the cause is unknown) is the most common form. It almost always occurs during a growth spurt just before and during adolescence. However, it can also occur in young children and even in infants. About 2% to 3% suffer from
Adolescents have a curvature of 10 degrees or more, but only about 0.3% to 0.5% have curves greater than 20 degrees. Mild curvature occurs equally in girls and boys, but curvature is 10 times more likely to occur in girls.
Medical risk factors. People with certain medical conditions that affect joints and muscles are more likely to develop scoliosis. About 10% of girls with Turner syndrome, a genetic disease common in women, develop scoliosis.
Young athletes. A 2000 study reported that young girls who did rhythmic gymnastics had a 10-fold greater risk of developing scoliosis. This elevated risk is likely due to three concurrent factors: an imbalance of weight on the spine, loose joints and a delayed onset of puberty. (Delayed menstruation is a common risk factor for all female competitive female athletes such as stress fractures and possibly scoliosis.)
Risk factors for the progression of curved scoliosis in affected children and adolescents
Once a mild curve is observed, the next step becomes more difficult, as it predicts whether or not the curve will progress to a more severe condition. Although as many as three in 100 teens have a condition that's serious enough to at least need observation, the likelihood of severity may be lower or above average depending on other factors.
• Being female or at a younger age at the onset of scoliosis increases your risk.
• The greater the bending angle, the greater the risk. At 20 degrees, only about 20% of the curves advance. However, young adults diagnosed with a 30 degree curve have a 60% risk of progression; With a 50 degree curve, the hazard is 90%.
• Girls who have low scoliosis and an unbalanced spine by more than an inch may be less likely to develop curves. Taller girls also appear to be at greater risk. Curvatures caused by congenital scoliosis (spine problems present at birth) may progress rapidly.
Risk factors for progression to scoliosis in adults
In rare cases, scoliosis may develop in adults who may have had unknown or untreated scoliosis in their youth. Osteoporosis or weak bones, a serious problem in many older adults, can cause mild curvatures to develop. (Osteoporosis itself is not a risk factor for the onset of new scoliosis.) However, in most cases, it is not known why adult curves progress.
How dangerous is scoliosis? Impact on the lungs and heart
The severity of scoliosis depends on the degree of curvature and whether it threatens vital organs, specifically the lungs and heart. Mild scoliosis effect (less than 20 degrees). Mild scoliosis is not serious and requires no treatment other than monitoring.
The effect of moderate scoliosis (between 25 and 70 degrees). It is still not clear if mild scoliosis causes major health problems. In one study, adults with mild scoliosis had normal lung function, although they had difficulty exercising.
The effect of severe scoliosis (more than 70 degrees). If the curvature exceeds 70 degrees, the severe twisting of the spine that occurs in skeletal scoliosis can cause the ribs to press on the lungs, restrict breathing and reduce oxygen levels. One study concluded that nearly two-thirds of patients with 90-degree curves and below had less than 80% of normal lung capacity. Abnormalities can also affect the heart and cause dangerous changes.
The effect of severe scoliosis (more than 100 degrees). Ultimately, if the curvature reaches more than 100 degrees, both the lungs and the heart can be injured. Patients with this level of risk are at risk of developing lung infections and pneumonia. Curves greater than 100 degrees increase the mortality rate, but this problem is very uncommon in America.
How is scoliosis diagnosed?
The severity of scoliosis and the need for treatment are determined by the extent of the curvature of the spine and the angle of rotation of the trunk (ATR). Both are measured in degrees. The two factors are usually related, so, for example, a person with a 20° spinal curve has a 5° ATR. This measurement used to be a standard for recommending treatment, although it is now known that up to 80% of 20° curves do not get worse. Scoliosis is diagnosed when the curve measures 11 degrees or more, but treatment is not usually required until the curve is 30 degrees and the ATR is 7 degrees.
physical examination
Forward bending test. A screening test often used in schools and in pediatric or primary care doctors' offices is called the forward bend test, in which the child bends forward with his arms hanging down, with feet together and knees straight. The curve of structural scoliosis is more pronounced when bending, and the examiner may notice an unbalanced rib cage, where one side is higher than the other, or other abnormalities. The forward bend test is not sensitive to deformities in the lower back, a very common site of scoliosis. Therefore, it misses about 15% of scoliosis cases, and many experts do not recommend this test as the only method for detecting scoliosis.
Other physical tests. The patient is usually asked to walk on the toes, then the heel, and then he is asked to jump up and down on one foot. These activities indicate leg strength and balance. The doctor will also check for tight tendons in the back of the leg, which is typical in adolescence, but may also indicate nerve root irritation or spondylolisthesis, a condition in which one vertebra slips forward over the other. The doctor will also check for nervous system dysfunction by testing reflexes, nerve sensation, and muscle function.
Recognize the curvature
Diagnosis
True is important, because poor judgment can lead to unnecessary X-rays and cumbersome treatments in children who are not at risk of progression. Unfortunately, although measurements of curves and rotation are useful, there is no test yet to determine whether or not a curve will advance. tilt (scoliometer). The clinometer (scoulometer) measures deformities of the trunk. The procedure is as follows:
The patient is asked to bend with outstretched arms and press the palms together, until a curve can be observed in the chest (upper back) area. The Scoliometer is placed on the back and is used to measure the apex (highest point) of the curve. Scoliometer results can indicate problems, and some experts believe it will be a useful tool for widespread screening. However, Scholetter's scales measure rib cage abnormalities in more than half of children who have been shown to have very little or no lateral curves. Scholetter's scales are not accurate enough to guide treatment, and if results show an abnormality, an X-ray should be performed.
Imaging tests
X-rays are currently the most cost-effective way to diagnose scoliosis. Experts hope that an accurate, non-invasive diagnostic technique can be developed that may eventually replace some of the X-rays currently used to monitor the progression of scoliosis. So far, some of these techniques appear to be fairly accurate for detecting scoliosis in the upper back (the thoracic region) but not scoliosis in the lower back (the woody region).
X ray. If the examination indicates scoliosis, the child may be sent to a specialist who takes an initial X-ray and monitors the child every few months with frequent X-rays. X-rays are necessary for the accurate diagnosis of scoliosis in several ways:
• X-rays reveal the degree and severity of scoliosis.
• An X-ray identifies any other abnormalities of the spine, including kyphosis (hunchback) and hyperlordosis (fluctuation).
• X-rays help the doctor determine whether the skeletal growth has reached maturity or not.
• X-rays of patients with curvature can help distinguish between structural and non-structural scoliosis.
Structural curves persist when a person bends, and non-structural curves tend to disappear. (It should be noted that sometimes muscle spasms or a growing spine can cause non-structural scoliosis, which shows a curve when bending.)
In children and adolescents with mild curvatures or in older adolescents with more severe curvatures, but whose growth has stopped or slowed, X-rays should be done every few months in order to detect the increased severity. Young adults with scoliosis should be sure to keep X-rays indefinitely in case back problems develop later in adulthood and need to be re-examined.
curve calculation
cup method. The degree of the curve is almost always calculated using a technique known as the Cobb method.
On an X-ray of the spine, the examiner draws two lines: one line that extends outward and upward from the upper vertebra edge of the curve. The second line extends outward and downward from the lower vertebrae. Then a vertical line is drawn between the two lines. The angle of intersection is measured to determine the degree of bending.
The Cobb method is limited because it cannot fully define the three dimensions of the spine. So they are not effective in determining spinal rotation or kyphosis. It also tends to overestimate the curve. Other diagnostic tools are needed to make a more accurate diagnosis.
A new technique that uses calculations based on geometric principles for the apex of the curve as well as the top and bottom of the curve to determine all dimensions of the curve may prove to be accurate.
Determine the end of growth
Even if the curve is calculated accurately, it is still difficult to predict whether or not scoliosis will progress. One way to predict whether or not the curvature will progress is to know when the child will stop growing. If a child has years to grow, the spine has more time to progress. If a child stops growing within a year, the progress should be very slight. (It should be noted, however, that some progression occurs in approximately 70% of the curves even after the spine has matured.)
Knowing a child's age is of course the first step in estimating the end of development. In addition, other methods have been developed to help predict the end of the growth phase.
One method is called the Risser's sign, which quantifies the amount of bone in the area at the top of the hip bone. A low score indicates that the skeleton still has significant growth; A high score means that the child has almost stopped growing and a small curve is unlikely to progress much further. The Rieser scale varies between genders and boys.
Scoliosis treatment has undergone significant changes over the past decade and a number of options are available.
treatment decision
The general rule for treating scoliosis is to monitor the condition if the curve is less than 20 degrees and consider treating curves greater than 25 degrees or those that progress by 10 degrees during monitoring. However, whether scoliosis is treated right away or just monitored is not an easy decision. The percentage of cases that will progress more than 5 degrees can be as low as 5% in certain cases and as high as 50% to 90% depending on severe curves or other predisposing factors:
• age. In general, the older the child, the less likely the curve will progress. Experts estimate that curves less than 19 degrees will progress by 10% in girls between the ages of 13 and 15 and 4% in children older than 15. (In some rare severe cases, the curvature may worsen even after treatment and the end of growth due to the pressure of body weight on the abnormal curvature.
• Gender. Girls are more likely to progress than boys.
• bending site
. Thoracic curves, those at the top of the spine, are more likely to develop from thoracolumbar curves or lumbar curves, those in the middle of the spine to the bottom.
• Intensity of bending. The higher the score, the more likely the lungs will be affected.
• The presence of other health conditions. Children in poor health may experience more stressful scoliosis treatments than other children. On the other hand, children with existing conditions that threaten lung and heart problems may need immediate and aggressive treatment.
معلومات عامة عن العمود الفقري
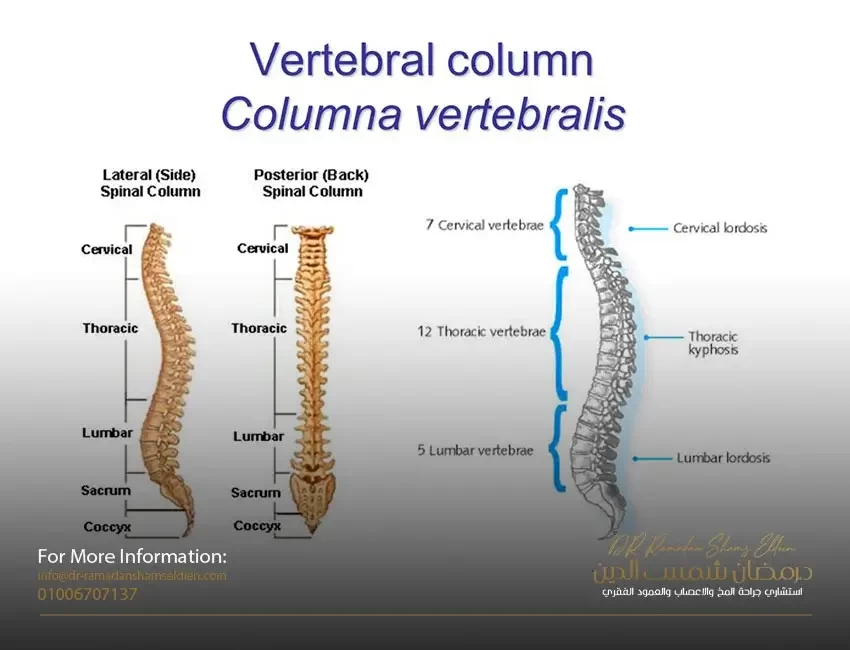
Backbones
The spine is a column of small bones or vertebrae that support the entire upper body. The column is grouped into three sections of paragraphs:
• Cervical vertebrae (C) are the bones of the cervical spine and consist of seven vertebrae that support the neck and head.
• The thoracic vertebrae (T) are twelve spinal bones connected to the rib cage.
• The lumbar vertebrae (L) are the five lowest and largest bones in the spine. Most of the body weight and pressure falls on the lumbar vertebrae.
• At the bottom of the lumbar vertebrae lies the sacral vertebrae, which is a skeleton in the form of a shield that connects to the pelvis at the sacroiliac joints.
• At the end of the sacrum there are two to four small vertebrae partially fused known as the coccyx or "tail bone".
• Each paragraph can be identified using a letter and a number; The letter reflects the region (C = neck, T = chest, L = lower back, and S = sacrum), and the number indicates its location within that region. For example, C4 is the fourth lowest bone in the cervical vertebrae, and T8 is the eighth thoracic vertebra.
• The vertebrae in the spine are separated from each other by small cushions of cartilage known as intervertebral discs, known to people as vertebral cartilage. Inside each disc is a gel-like substance surrounded by a fibrous structure. The disc is 80% water, which makes it very flexible.
• Each vertebra in the spine contains a number of bony projections, known as processes. Spinal processes and transverse processes are connected to the muscles in the back and act like little levers, allowing the spine to twist or bend. The articular processes form the joints between the vertebrae themselves, they meet together and intertwine.
• Each vertebra and its processes surround and protect a central opening in the form of an arch. These arches, aligned down the spine, form the spinal canal, which surrounds the spinal cord, the central stem of the nerves that connect the brain to the rest of the body.
• The upper torso usually has a gentle external curve (kyphosis) while the lower back has a reverse internal curve (lordosis).
كل ما تود أن تعرفه عن الغدة النخامية
the pituitary gland
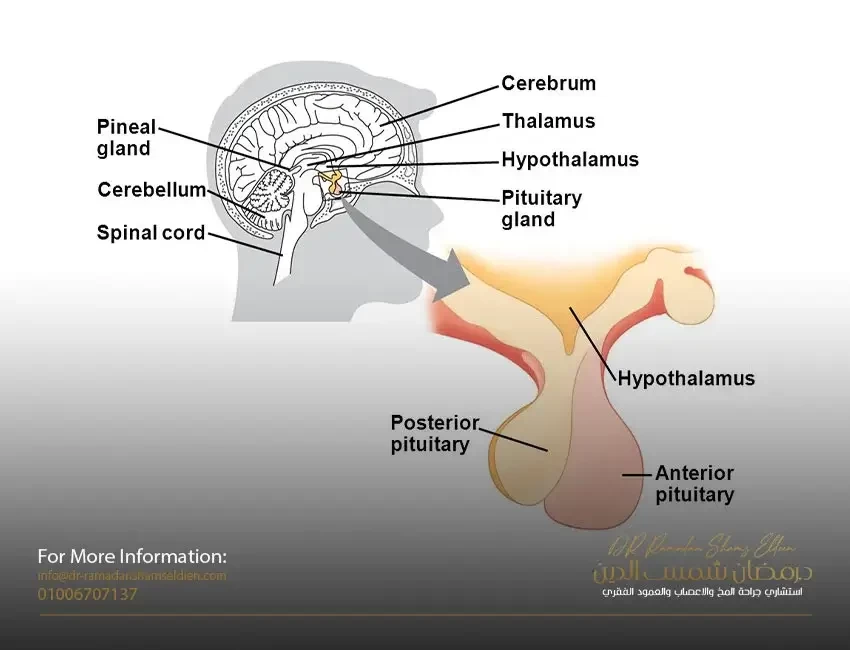
It is a very small gland located in the middle of the bottom of the skull, its diameter is not more than 1 cm and its weight is between 1/2 to 1 g
It is located in a small bony cavity known as the saddle above the sphenoid sinus at the bottom of the skull.
Before the twentieth century, it was prevalent among scientists that its function was to drain pituitary secretions from the brain through the nose.
With the beginning of the twentieth century, its role in hormonal control in the body was discovered, and after that, the discovery and separation of the hormones generated from it and its chemical composition and its role in controlling other tissues, organs or glands in the body.
In the middle of the twentieth century, the regulatory relationship of the so-called hypothalamus with the pituitary gland was discovered, and it was a new beginning to understand the movement of hormones in the body, and that all endocrine glands are linked to the pituitary gland and the pituitary gland is directly linked to the brain through what is known as the hypothalamus.
• What is the function of the hypothalamus?
• It secretes two groups of hormones, one of which stimulates the pituitary gland and the other inhibits it
• It also contains the bodies of neurons that control the posterior lobe of the pituitary gland
Which consists???????
It consists of two parts, the anterior lobe 2/3 of the pituitary gland, which is a glandular tissue that secretes hormones
Posterior lobe 1/3 of the pituitary gland It is a nervous tissue that contains nerve endings that transmit hormones.
• When a disorder occurs in the pituitary gland, it leads to a disorder of the body as a whole in one way or another, due to the loss of the balance that we talked about earlier.
• Syndrome known as menopause or disorder and increased milk secretion.
• Of course talking about the main or central cause associated with the pituitary gland.
• Because there are many reasons for the increase in the milk hormone leading to this pathological syndrome, known as peripheral causes. (Pregnancy, breastfeeding, medications, muscle stress, psychological disorder, laziness of the thyroid gland)
The central or main reason for the increase in the milk hormone is the increase in the size of the pituitary gland due to a benign tumor in it or the hypothalamus or any pressure on the arm that connects the hypothalamus to the pituitary gland.
The most famous is pituitary adenoma
• What are the symptoms?
• In females: menstrual irregularities, constant presence of milk in the breasts, primary or secondary infertility, low sexual desire.
• In males: primary or secondary infertility, impotence, pathologically increased breast size.
• General symptoms due to direct pressure at the site of the tumor: headache, vomiting tendency, dizziness, disturbance of the field of vision, and other hormonal imbalance.
treatment
• Pregnancy: Pregnancy causes the pituitary gland tumor to shrink.
• Staying away from psychological disorders and stress, because in their presence the secretion of the milk hormone increases.
• Avoiding muscular stress in women.
• Medications: There are drugs that cause the pituitary gland tumor to shrink. Most cases of the pituitary gland leading to increased milk hormone respond to drug therapy.
Surgical intervention: In the event of symptoms resulting from direct pressure on the optic nerve, hypothalamus and vital brain tissues, direct and rapid surgical intervention is recommended.
In the case of surgical intervention, it is microscopic surgery or endoscopic surgery through the nose.
القيلة المائية الظهرية - أنواعها وكيفية علاجها
Hydrocele or myelomeningocele
It is one of the common birth defects in our societies. It is usually diagnosed during pregnancy and is dealt with in the first days immediately after birth by doing CT scans and magnetic resonance imaging of the brain and spine. Whereas, based on the results of these tests, the diagnosis is confirmed and treatment methods and priority are determined. It is an opening in the vertebral column, which occurs when the process of closing it is not completed during the stages of embryonic development. Where the membranes surrounding the spinal cord appear outside the open vertebra, and some of the nerve-coated parts of the spinal cord emerge from the back, from the back.
Types of meningocele
1. Meningomyelocele. It is the exit of the contents of the nerve bag represented by the nerve roots with the surrounding membranes from the posterior opening of the affected vertebra. It is possible for this cyst or hydrocele to explode during childbirth with the exit of the cerebrospinal fluid, or the cyst is covered with a dark or incorrect layer of skin.
2. Meningocele. It is the emergence or emergence of a posterior cyst against the incomplete vertebra and it contains cerebrospinal fluid only. Also, this cyst or hydrocele may explode at birth with the exit of the cerebrospinal fluid, or the cyst is covered with a dark or incorrect skin layer.
3. Another case is myeloschisis. A condition in which the back skin components of the spine and the membranes are completely missing, and if we look at the back we see the spinal cord completely exposed.
Consequences of having a meningocytosis
1. Dysfunction in the nervous ability to move the lower extremities
2. Deformation of the feet or legs
3. Weakness or loss of superficial sensation in the lower extremities
4. Poor or no control over the two excreting processes
5. Intellectual performance - In general, most children with unaccompanied myelomeningocele do not have any impairment in mental functioning. But in some cases, a number of them have learning difficulties.
treatment
The obstetrician and gynecologist supervising the birth of such cases calls the neurosurgeon immediately after birth because the incision is open, it is possible for fluids to leak from the brain, and cause pollution in the central nervous system. Therefore, surgery is performed on the child during the first or second day after birth from order to close the incision. During the surgery, the incision in the back is closed, preventing fluid leakage and infection. However, the surgery does not reduce the condition of the paralysis or even the nerve damage that occurs in the part at the level of the incision and below it. It also needs to be followed up by a urologist, as many of these children need a diversion to the urethra. Children with spina bifida can lead normal and active lives. Also, most of them can walk reasonable distances with the help of a leg brace. But most likely these children will also need a wheelchair to get around. The extent of disability is related to the height and position of the affected vertebra.